Warning: Invalid argument supplied for foreach() in /home1/redcare1/public_html/wp-content/themes/uplift/swift-framework/content/sf-post-formats.php on line 89

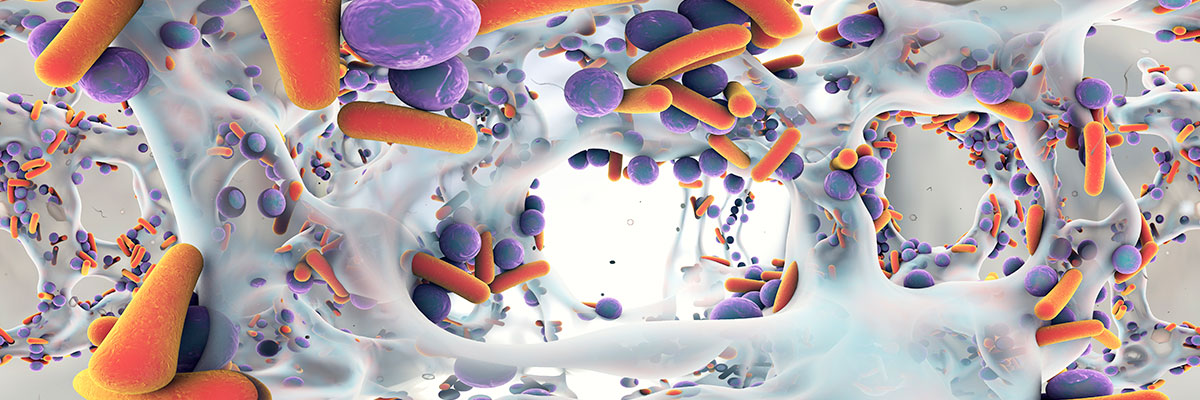
Antibiotics are medicines used in preventing and treating bacterial infections. Antibiotic resistance occurs when bacteria change and adapt in response to the use of these medicines thus rendering them ineffective. Antibiotics resistance is one of the biggest threats to global health, food security and development today. It can affect anyone of any age and in any country. Every year, at least 700,000 people around the world die from infections with superbugs that are resistant to antibiotics – and this is predicted to rise to 10 million by 2050.
A growing number of infections like pneumonia, tuberculosis and gonorrhea have become more difficult, and sometimes impossible to treat. Antibiotic resistance leads to longer illnesses and hospital stays, higher medical costs, and more deaths. At the same time, not enough new antibiotics are being developed to replace older and increasingly ineffective ones.
The current global antibiotic resistance crisis is the result of many factors including:
- Over-prescribing & dispensing of antibiotics
- Misuse and overuse of antibiotics by patients
- Lack of new antibiotics being developed
- Poor infection control in hospitals, clinics and surgical theatres
- Lack of toilets & proper sewage disposal
In places where antibiotics can be bought without a prescription, the emergence and spread of resistance is made worse. Similarly, in countries without standard treatment guidelines, antibiotics are often over-prescribed by health workers and over-used by the public. Without urgent action, we are heading for a post-antibiotic era, in which common infections and minor injuries can once again easily kill.
Steps can be taken at all levels of society to reduce the impact and limit the spread of resistant infections, and there is a role for everyone to play:
- First, an awareness that not every condition requires antibiotic; not every cough or wound is due to bacteria, and using antibiotic might constitute abuse
- Only use antibiotics when prescribed by a certified health professional.
- Never demand antibiotics if your health worker says you don’t need them.
- Always follow your health worker’s advice when using antibiotics.
- Never share or use leftover antibiotics.
- Prevent infections by regularly washing hands, preparing food hygienically, avoiding close contact with sick people, practicing safer sex, and keeping vaccinations up to date.
- Prepare food hygienically, following the WHO Five Keys to Safer Food (keep clean, separate raw and cooked, cook thoroughly, keep food at safe temperatures, use safe water and raw materials) and choose foods that have been produced without the use of antibiotics for growth
- Always complete the course of any antibiotic treatment prescribed to you, even if you feel better before finishing them

To prevent and control the spread of antibiotic resistance, health professionals can:
- Prevent infections by ensuring your hands, instruments, and environment are clean.
- Only prescribe and dispense antibiotics when they are needed, according to current guidelines.
- Report antibiotic-resistant infections to surveillance teams.
- Talk to your patients about how to take antibiotics correctly, antibiotic resistance and the dangers of misuse.
- Talk to your patients about preventing infections (for example, vaccination, hand washing, safer sex, and covering nose and mouth when sneezing)

It is not too late to reduce the impact of antibiotic resistance. We all have a part to play in preserving the effectiveness of antibiotics by having a different and well informed attitude, preventing the spread of infections and changing how we prescribe and use these medicines.
- Umar Adegoke



